Family carers: Northern Ireland is lagging

agendaNi looks at the current push to support informal carers in Northern Ireland, a valuable resource to health and care services delivery which is facing increasing pressures, to align with changes across the rest of the UK.
It’s estimated that there are close to 214,000 informal carers in Northern Ireland providing at least 2.4 million hours of unpaid work every week. A total of 12 per cent of the population carry out some form of informal caring, for which the Government would otherwise have to pay £832 million a year at the minimum wage rates.
While across the UK legislation has been introduced which addresses carers’ rights, Northern Ireland has lagged behind. It has long been recognised that the current care model would be unsustainable without informal carers, but also that demographic and socio-economic trends is putting greater pressure on informal carers as a resource.
The definition of an informal carer is a person, usually unpaid, who care to someone with long lasting health or care need, outside a professional or formal employment framework. Informal carers ‘prop up’ the formal care systems, not just in the UK but across the world. It is estimated that 80 per cent of all care across the European Union is given by family and friends.
Issues such as the impact of caring on a person’s physical and mental health, the impact of their lifestyle outside of caring, financial difficulties due to confliction with paid work commitments and education/career prospects, are some that have been raised as not being addressed for carers in Northern Ireland.
Although a clear need to support carers has been established, the last legislative change in Northern Ireland took place back in 2002 in the form of the Carers and Direct Payments Act (Northern Ireland). This piece of legislation gave carers the right to an assessment and to be considered for services to meet their assessed needs.
It placed a duty on Health and Social Care Trusts to inform carers of their right to a care assessment and the right to provide personal social services to support carers directly. However, Trusts retain discretion to decide whether or not to provide service(s) to meet a carer’s identified needs.
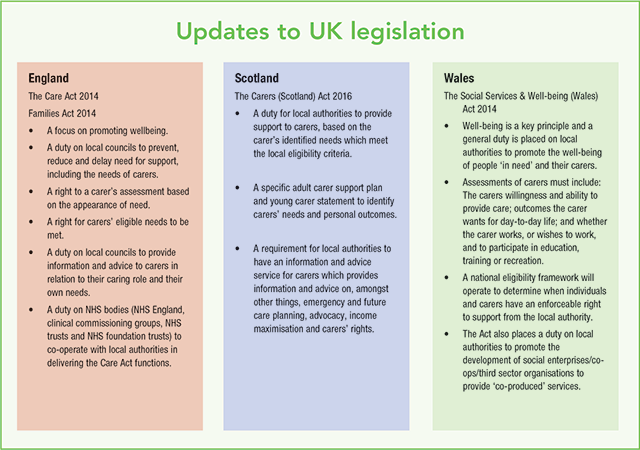
The most recent strategy for addressing carers’ issues for Northern Ireland, Caring for Carers (2006) is now over 12 years’ old, compared to The Care Act 2014 and Children and Families Act 2014 in England, the Carers (Scotland) Act 2016 and The Social Services and Well-being (Wales) Act in 2014.
Taking The Care Act as an example, it’s key features were the introduction of a duty on local authorities to provide the services required, within a national eligibility criteria. Also, it broadened the criteria for respite care to allow carers to engage in work, training, education, volunteering or recreation.
An updated edition of the scheme was published in March 2016 following a review of its implementation and took account of regulatory changes, feedback from stakeholders and the care sector, and developments following the postponement of social care funding reforms to 2020.
In 2014, the Northern Ireland Human Rights Commission (NIHRC) made a series of recommendations in relation to the human rights standards for carers. They proposed:
- Giving specific consideration to the needs of older carers and child carers – for the latter to introduce a child carer assessment, educational initiatives and the creation of a statutory duty on educational bodies to support young and student carers;
- NI Executive programmes aimed at alleviating poverty should take full account of challenges faced by carers; and
- Enhancement of legal protections for carers seeking the right to work.
While no legislative changes have been made in Northern Ireland, ongoing work to reform adult care and support in Northern Ireland has to some degree recognised the need to establish the rights of family carers in Northern Ireland on a legal footing and to establish a carer-centred strategy. However, assessing and potentially implementing these changes is currently being delayed due to the absence of a minister for health.
Development to support carers in Northern Ireland, via either policy or law changes, will require further work. The OECD recently identified three key areas for support policies for carers. These are:
- Helping carers combine care responsibilities with paid work;
- Improving carers’ physical and mental health and wellbeing; and
- Compensating and recognising carers.
It is likely that any legal or policy changes in Northern Ireland, when it is made, will take place in these areas. However, the form of these changes will require further consultation and ministerial direction. While proposals for change may take various forms, undoubtedly, the underpinning reason for change must be to acknowledge, recognise and value the role of informal carers.
This article was formed, with approval, on the basis of the ‘Supporting carers in Northern Ireland: Where are we with legislation and policy to support them?’ blog, which appeared on the Northern Ireland Assembly’s Research and Information Service (RaISe), authored by Dr Janice Thompson.