Restructuring of planning
 The devolution of planning powers to the 11 local councils and the subsequent creation of the Department for Infrastructure (DfI) created a new planning system for Northern Ireland and re-distribution of planning functions. While responsibility for planning is defined as shared between local councils and the Department, the bulk of functions have been taken on by planning committees within the councils.
The devolution of planning powers to the 11 local councils and the subsequent creation of the Department for Infrastructure (DfI) created a new planning system for Northern Ireland and re-distribution of planning functions. While responsibility for planning is defined as shared between local councils and the Department, the bulk of functions have been taken on by planning committees within the councils.
Here are the new roles, as outlined by the Department and their potential benefits.
The 11 local councils are responsible for:
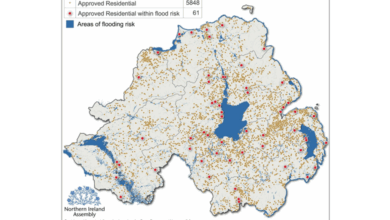
- Local development planning: creating a plan which will set out how the council area should look in the future by deciding what type and scale of development should be encouraged and where it should be located;
- Development management: determining the vast majority of planning applications;
- Planning enforcement: investigating alleged breaches of planning control and determining what action should be taken.
DfI Planning is responsible for:
- Determination of regionally significant applications and ‘called-in’ applications;
- Regional planning policy;
- Planning legislation;
- Regional Development Strategy (RDS);
- Oversight and guidance for councils;
- Performance management;
- Crumlin Road Gaol & St. Lucia Barracks.
Benefits
- Local decision making: local councillors know their environment, needs and views of local people and so are best placed to make the decisions on how their area should grow and develop;
- Meeting local need: councils will make planning decisions suited to local communities and will have greater freedom to respond to local need. They will also be able to ensure that the needs of local businesses are taken into account which can help create jobs and growth in the local economy;
- Community involvement: the local development plan allows councils to discuss plans and planning applications with local communities earlier and more meaningfully. This gives business, communities, groups and organisations a real opportunity to have a say in shaping their local area.
Under the new planning process applications are now classed as local, major, which are the responsibility of councils, and regionally significant, which falls under the Department’s remit. While the council’s planning committee will be responsible for the majority of decisions such as large developments, contentious applications and those that receive a number of objections, each council will publish a Scheme of Delegation, setting out which applications will be dealt with by the committee and which will be delegated to officers. Also, each council also has its own planning office, which will deal with queries and issue advice.
DfI’s planning functions have recently relocated to Adelaide Street in Belfast.