Education
New political composition of the Education Authority Board
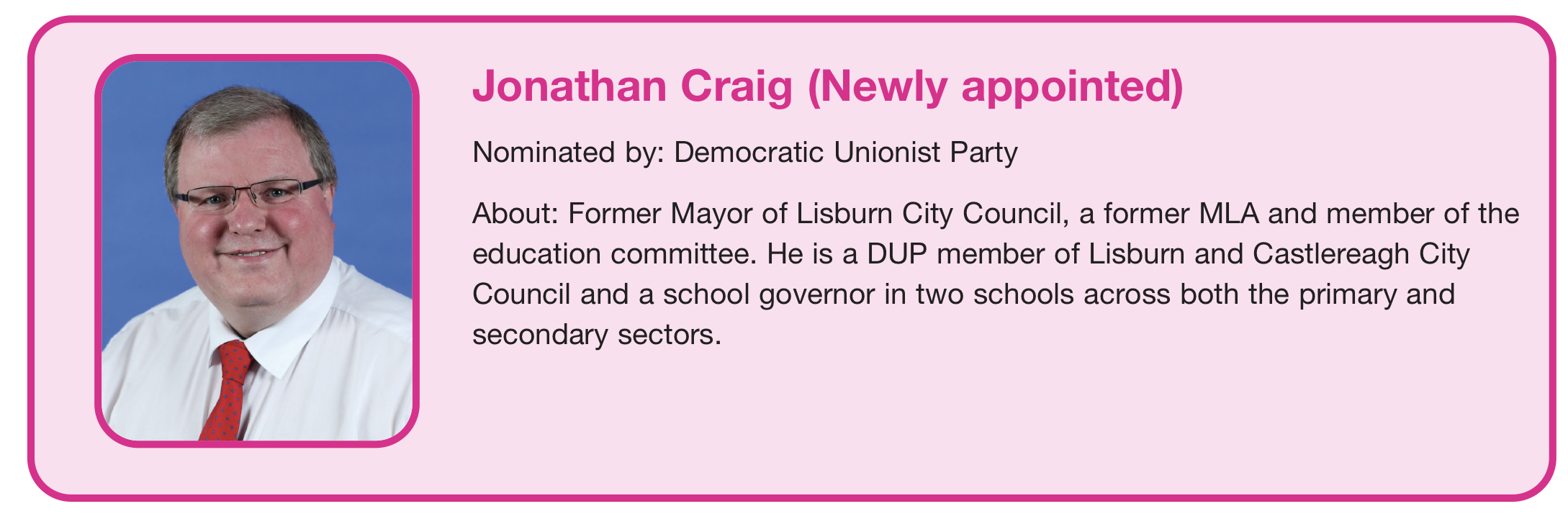
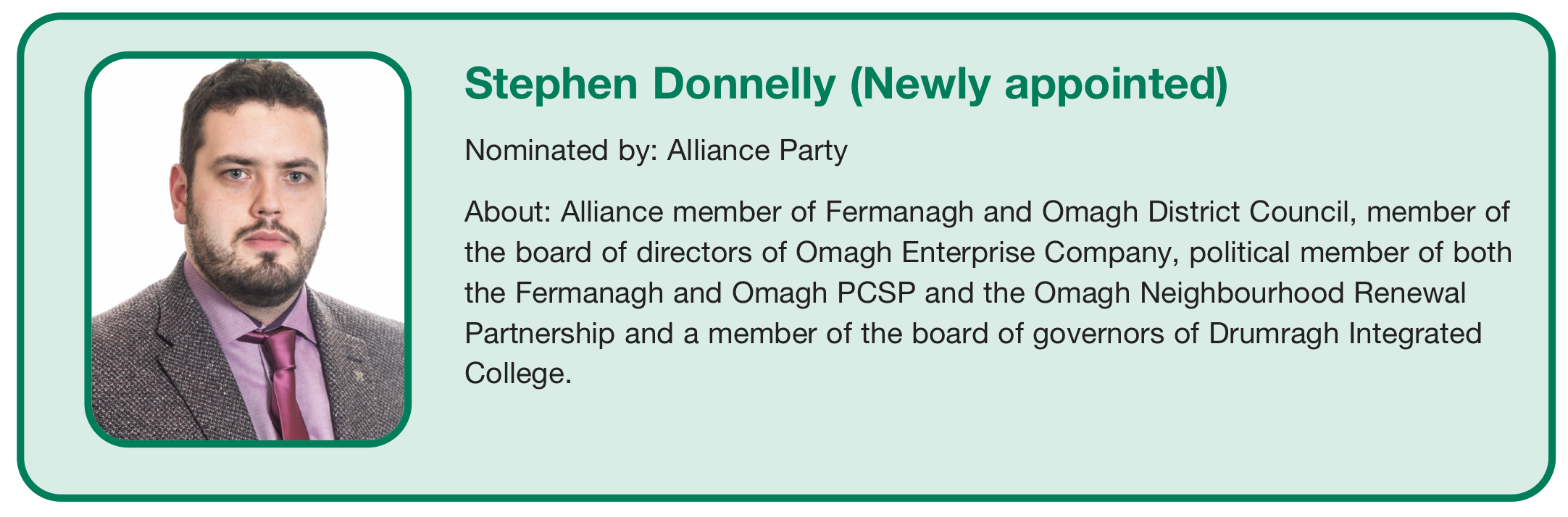
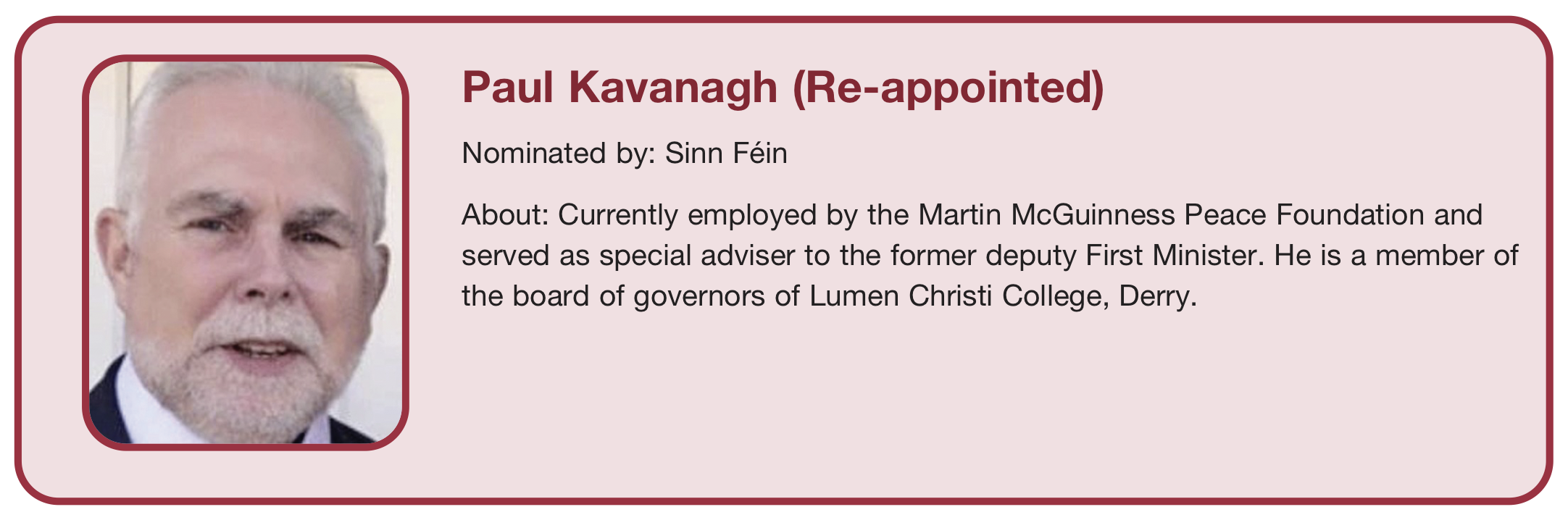
There have been four changes in the political makeup of the Education Authority board following May’s Northern Ireland Assembly elections.
The board is made up of 20 members, eight of whom are political nominees. The membership is allocated using the D’Hondt method. This allocated three seats to Sinn Féin (no change), two to the Democratic Unionist Party (down one), two to the Alliance Party – who had previously been unrepresented – and one for the Ulster Unionist Party (no change). The SDLP lost their sole seat on the board.
The remaining are non-political appointees. Twelve members represent other interests like the Irish medium sector, grammar schools, and the main churches in Northern Ireland.