Round table discussion: Optimising patient waiting lists with AI

eir evo hosted experts from the health and tech sectors for a round table discussion on optimising patient waiting lists with AI.
How can digital tools and AI best support the Encompass programme and help staff and patients get the most value from it?
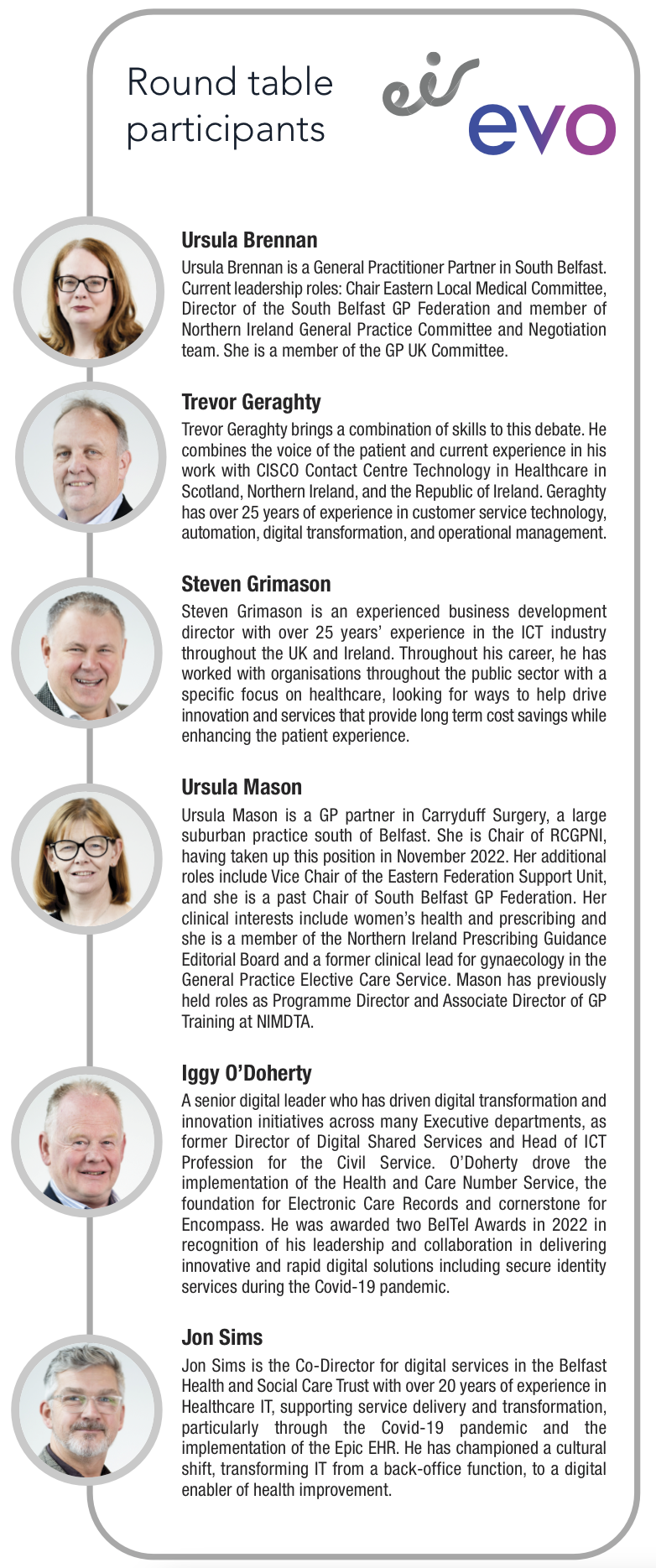
Ursula Mason
General practice does not interface with Encompass in the same way as the rest of the system, and this is a challenge. Patients rely heavily on GPs because we hold the entirety of their record, from cradle to grave. The interface between Encompass and the GP IT system must be made more robust. We must have interoperability between both systems to enable seamless communication for patients. The My Care app works for digitally literate people, but those who are not, often ask their GP for some of the information the app provides. Digital tools and AI can be used to address this, but it is about trying to fit the right tool to the right patient.
Iggy O’Doherty
Encompass has transformed the health service IT infrastructure. AI can help the service take a quantum leap forward. System-wide data in the healthcare system must be exploited, not just by separate entities, but from primary and secondary care. Digital tools and AI alone will not help; we must develop skills and capability while fostering collaboration between the public and private sector. There has been significant uptake in the My Care app, and it is a good start, but there is much more that can be done. Currently, the use of AI is being rolled out piecemeal. We need a health AI strategy to establish governance and ethical approach, drive consistency of use and prioritise key areas where we can drive maximum value.
Jon Sims
An AI strategy is crucial but there is no ‘one-size-fits-all’ for AI deployment as not all deployments will be scalable, but AI will be beneficial and must be service- led as the patient must be at the heart of these conversations, and each approach must also link with the organisational and regional strategy. We must recognise we only are 15 months into the Encompass journey for Belfast and going live is the starting point, not the finishing line. It is still in the stabilisation process where we assess progress, consider what works, and identify areas for improvement.
Trevor Geraghty
There is a lot being done in Northern Ireland which is to be celebrated. The My Care app has changed people’s lives and understanding. This creates an opportunity to get the population more engaged with a constrained health service. Digital tools that are successful need to be built on. It is an iterative process, and it is essential that we continuously assess the journeys. If we are testing technology, we can and should do so quickly.
Ursula Brennan
Trevor has mentioned the positive around population engagement through My Care. In my opinion, the digital innovation has been brilliant for some but not all. Many do not have the requisite skills to use devices or understand the information. The speed of change is now so rapid. We need to understand how patients, clinicians, and staff catch up and keep up. Constructing and developing Encompass and Epic to create something that best suits all our needs is going to take time.
Ursula Mason
It is critical we support people who struggle with digital communication, so they are not left behind or discriminated against. We must recognise that we have the highest level of health inequality across these islands. One-in-three people live in the highest quintile of deprivation here. They may not be digitally enabled and may not have a level of health literacy that allows them to get the most from this type of communication. Whatever we do regarding patient care, we must have both digital and non-digital solutions that do not exacerbate the health inequalities that already exist.
Steven Grimason
Services are extremely good once you get into them. Encompass is helping to transform the sector but the blocker that remains is how we access the services. We must be more inclusive. It is easier for people to interact with services such as Amazon than it is for people to book a GP appointment. We need to assess how we can make it easier for people to access our health services.
Ursula Brennan
GPs just do not have the capacity to offer that speed of an ‘Amazon’ style service. This is only partly because GPs are performing functions that could be digitalised. When we look at developing digital innovation strategies we must remember what we still do not have in place. Northern Ireland still does not have E-prescribing which makes us an outlier in UK and Ireland. This is a digital innovation that would release time tomorrow.
Should HSCNI give patients more choice in how they communicate to secure digital channels?
Iggy O’Doherty
The challenge is building a hybrid model. I do not believe it is a digital-only solution that we need to deploy across the health service. We need to consider good governance, ethics, quality, confidentiality, and data protection. Every patient is different; some are proficient with technology through portals and apps, SMS, text, and emails. However, some are not and we also need to me mindful of demographic changes regarding age, spoken language, and ability. The key is flexibility; we must ensure that services are accessible to all, using digital options for those who need them, but ensuring that people’s needs are met across all mediums.
Jon Sims
We need to strike the balance between patient choice and security within these patient channels considering data management provisions and GDPR protections. It is about having a comprehensive range of options for patients, and the more comprehensive the spread, the more supported people will be. Ultimately, it is a balancing act between increasing accessibility and doing it securely. Anything we put in place has to be scalable and supportive to the population. There can be choice, but we have to ensure it is balanced and secure, taking some of the factors that Iggy has mentioned into account.
“Northern Ireland needs an AI strategy for health, and it is crucial we invest in data analysis.”
Iggy O’Doherty
Trevor Geraghty
You have to meet people where they are, and inclusion is the most important factor. With AI and technology, we are at a point where we have options to create real change for the very first time. So we should roll out these new innovations while retaining traditional models in order to ensure accessibility for all. There are going to be cohorts of the population who require additional support, and we must ensure that services account for this. Overall, the answer to the question is yes, as long as they are secure and accessibility for all is maintained.
Ursula Brennan
It is absolutely essential that any and all of the digital aspirations being discussed here bring people along. We must be mindful of how we engage with all sectors. We should increase choice for patients as long as the health sector has the capacity to manage the outworkings of that, which are governance and safety. Self-care is important for all of us; we are living in a cash-starved environment where our waits are long, but enhancing self-care and preventative medicine can reduce reliance on accessing health care services in the first place.
Steven Grimason
It is about having models which are fit for the future. Studies show that nearly every person under the age of 25 is tech literate, so that is what the services of the future must account for. One-in-10 people do not read letters, so we cannot just continue to send letters when this is not the best means of meeting people’s needs. Over 80 per cent of people use WhatsApp; these are just the facts. The key to having services for the future is having flexibility in how we communicate and provide services.
Ursula Mason
Choice is important, because we have a society where there is not equity of access. If we are going to create more digital channels, we need to account for all of the needs that have been mentioned such as safety, data protection, and security. Apart from self-referral services, if you are on a hospital waiting list, another human has referred you. If you are a GP or another medical professional who delivers care for patients, you are someone whose capacity is finite. Change needs to meet people where they are and we need to create equitable solutions. We must be careful to not inadvertently reduce access by having too many channels.
Could an AI-driven contact centre improve access to care and reduce pressure on staff by offering 24/7 support?
Steven Grimason
AI could completely transform how patients and staff interact with health services. A 24/7 AI-driven contact centre would mean staff could instantly access HR or payroll without waiting for office hours, while patients could manage appointments and access services more easily. For example, if someone cannot attend an appointment, they could reschedule or cancel through WhatsApp or another smart platform, and that slot would automatically return to the system for someone else, reducing waste and delays. AI could also remove barriers for those who do not speak English by translating text or voice interactions. Patients could see available times, confirm appointments, and even receive GPS directions or maps to hospital departments. This creates a seamless, interactive experience that is secure, multilingual, and always available. This vision does not remove human connection, it enhances it. Patients could choose to speak to a person at any stage. My ‘utopia’ is a health service where AI supports both staff and patients, improves communication, and eliminates inefficiencies like unanswered calls, lost letters, or long waits. With the right governance and security, there is no reason we cannot embrace AI to make healthcare more responsive, connected, and compassionate.
“We must have both digital and non-digital solutions that do not exacerbate the health inequalities that already exist.”
Ursula Mason
Ursula Brennan
AI could greatly improve communication and reduce inefficiencies. Clinicians waste significant time answering queries about waiting lists and referrals due to limited visibility of real-time information. An AI system could give patients accurate updates, empowering them to make informed choices about their care. It could also support staff productivity by providing 24/7 assistance for issues like IT or payroll, particularly outside normal hours. With appropriate governance, confidentiality, and safety frameworks, AI could enhance both patient journeys and clinicians’ working conditions, ensuring timely information, reduced frustration, and better use of valuable clinical time.
Jon Sims
AI is not about replacing human interaction, but removing repetitive, low-value tasks like appointment booking or FAQ responses. Using natural language processing, AI could guide patients to the most appropriate pathway, whether that is a clinician, administrator, or automated response. This benefits both patients and staff, especially as healthcare increasingly operates around the clock. With systems like Epic EHR, staff often face access issues out of hours; AI could help resolve these instantly. By automating routine processes, we can free skilled professionals to focus on meaningful tasks and improve patient care efficiency.
Iggy O’Doherty
AI, by its nature, can provide 24/7 support. It could triage patients based on symptoms, directing them to the right service or person. Beyond typical contact centre functions, AI can rapidly answer complex queries by linking multiple datasets, for example, providing transport options, appointment details, or care pathways. This integration across health and public data systems would enhance accessibility and responsiveness, giving patients immediate, accurate information while reducing administrative burdens on staff. Essentially, AI offers faster, more connected, and more comprehensive support than traditional contact centre models.
“There is huge potential to reduce missed appointments through smarter communication.”
Trevor Geraghty
Trevor Geraghty
AI can significantly improve access and relieve pressure on staff. Two approaches exist: fully automated AI agents that handle entire interactions, and AI assistants that support human operators. Both can reduce queues and improve responsiveness. Crucially, AI can also monitor staff wellbeing, identifying stress patterns before burnout occurs. As AI handles simpler queries, humans will face more complex cases, so supporting them with intelligent systems is essential. Properly deployed, AI ensures patients and staff receive timely, effective support, improving service quality while protecting workforce wellbeing.
Ursula Mason
AI offers great potential for process-driven tasks like appointment management, reducing missed appointments, and increasing flexibility. It can simplify navigation for patients, improving accessibility for those who struggle with complex systems. However, I am cautious about AI in clinical triage or decision-making. Current evidence on bias, accuracy, reliability, and hallucinations within products is not yet robust enough for full clinical deployment. As clinicians, we must ensure AI tools meet the same evidence and safety standards as medicines or procedures. With strong governance and evidence, AI can enhance care safely, but for now, it is best focused on administrative and logistical support.
How can smarter communication and digital engagement help reduce missed or cancelled appointments?
Trevor Geraghty
There is huge potential to reduce missed appointments through smarter communication. Traditional letters often fail for people with unstable addresses or busy lives, so using digital reminders and education can make a major difference. AI could ensure patients know when appointments are, what preparation is required, and what to do in advance. For example, someone waiting years for surgery might not realise they must meet certain health criteria first. Consistent digital engagement could guide and motivate them to be ready when called, preventing wasted appointments and ensuring that limited clinical time is used effectively.
Ursula Mason
Improving communication makes the patient journey more efficient and rewarding for both patients and staff. Missed appointments waste scarce capacity and frustrate clinicians. Smarter systems could give patients real-time updates on where they are on waiting lists and allow them to cancel or confirm easily. Better engagement also helps identify those who no longer need appointments, freeing space for others. Regionally linked communication tools could prevent letters being missed and ensure that every slot is used. Fundamentally, it is about maximising the capacity we already have and supporting people to stay connected to their care pathway.
“AI could greatly improve communication and reduce inefficiencies.”
Ursula Brennan
Ursula Brennan
Missed appointments often happen because of poor communication, not lack of willingness. Simple digital tools, like automated text reminders, could dramatically reduce ‘did not attend’ rates, but many practices lack funding to implement them. These systems need to be consistent and equitable across the NHS, not just in larger, better-resourced facilities. If supported properly, reminders and two-way digital communication could save significant time and improve patient outcomes. Investment in basic, universal digital engagement would pay dividends in reducing waste and ensuring all patients, regardless of location, receive timely, effective reminders.
Jon Sims
This is not a scheduling problem, it is a communication problem. Missed appointments happen when patients do not receive or cannot respond to reminders. AI could use predictive modelling and data to identify patients likely to miss appointments and trigger flexible rescheduling. Communication must be two-way, allowing patients to confirm, change, or cancel easily. However, not everyone is digitally active, so multiple communication options are vital. By improving digital engagement, using reminders, and reallocating freed slots dynamically, we can make far better use of existing capacity without overburdening the system or excluding non-digital users.
Iggy O’Doherty
Automated reminders via mediums such as text, email, or apps are essential, not optional. Two-way communication builds trust, allowing patients to confirm or cancel appointments quickly. Personalised messages, delivered in a patient’s preferred language or format, improve attendance. AI could also help tailor appointment times, for example, offering later slots to those travelling long distances. Regional, connected systems across primary and secondary care would ensure consistency and reduce duplication. By giving patients easier access to booking, confirmation, and their own health information, we make care more flexible, inclusive, and efficient for everyone.
Steven Grimason
AI could clean up waiting lists and improve engagement. Many people remain on lists unnecessarily because no one checks if they still need care. Smart messaging through platforms like WhatsApp could easily ask: ‘Do you still need your knee consultation?’ A quick reply could remove outdated cases, giving a more accurate view of demand. This approach also allows flexible, private communication, especially for mental health patients who might find phone calls difficult. Fundamentally, healthcare should be as intuitive to access as online services, flexible, compassionate, and built around people’s real lives.
Ursula Brennan
Managing ‘did not attend’ (DNA) cases could also be streamlined. Currently, letters are sent back to referrers, creating extra admin work. If DNA communication were handled directly through the referral hub or AI system, patients could be automatically notified and re-engaged sooner. This would save time, reduce delays, and ensure referrers remain informed without adding manual workload. Smarter automation would allow the system to handle these routine follow-ups quickly and consistently, freeing clinical teams to focus on patient care rather than administrative tasks.
Jon Sims
Preventing DNAs is ideal, but when they do happen, automating the response and removing repetitive manual tasks keeps the system efficient. We need to focus human effort where it adds value, not on chasing missed appointments that technology could easily manage. Smarter communication reduces both missed opportunities and wasted effort.
“We need to focus human effort where it adds value, not on chasing missed appointments that technology could easily manage.”
Jon Sims
Ursula Mason
We should focus on enabling attendance, not just reducing DNAs. If referral systems capture patients’ needs like mobility, transport, or language barriers, AI could automatically coordinate supports, such as transport booking or translation, when appointments are scheduled. Over time, this builds a patient profile that ensures consistent, accessible communication across services. Meeting patients where they are, rather than expecting them to adapt to the system, would make attendance easier, fairer, and more efficient for everyone.
What digital solution can best help GPs and community services work more efficiently while improving the patient experience?
Ursula Brennan
Accurx has revolutionised the way I work. It is an SMS tool that allows me to easily share vital information with patients including referrals and booking links. I could not live without it now. Our patient population absolutely love it.
Iggy O’Doherty
I think we should expand telemedicine and virtual care services. It has been widely adopted here and allows people to consult with GPs remotely. That reduces travelling time and increases access to care. There is also GPIP, the General Practitioner Intelligence Platform. It combines data from all GP practices and can be utilised to provide a regional view.
Ursula Mason
Robust data coding is essential to improving the health and wellbeing of our population, while reducing health inequalities. For the last 20 years, GPs have amassed a really rich dataset. This must now be connected with the data being collected through Encompass. However, both must be aligned and that is a significant challenge. To move from a sickness service to a health service, we must consider prevention. If we use appropriate data to take a whole system population health view, it would allow the development of interventions that would have the greatest impact on the health of our population.
Jon Sims
Maintaining people’s health is critical, but people do not engage with the health service unless they are unwell. There is an absence of preventative measures. We have the opportunity to move from a reactive to a proactive health service. We must use digital solutions that address the need for people to present to the health service in the first place.
Trevor Geraghty
GPs have an unlimited amount of agreed currency, it is called trust. Most people trust their GP. We can use this trust, enabled by technology, to educate people on what health problems they should look out for. Telemedicine can be used to enhance the patient-initiated follow-up. We must also assess the entire journey of an appointment for a patient. This includes simple things such as where they must go, and where they can park. Trusts are constantly receiving calls for simple queries like this and it constrains resources. Technology can resolve this.
Steven Grimason
It is great to have GPs and the health service together because it is a single health service, it is a single journey. However, citizens’ view is that it is a little broken and disjointed at times. I believe AI enables us to combine datasets in the way in which Ursula [Mason] spoke about. There are ways in which we can safeguard this so only the people who should see it can see it. The technology is there and using it will save money, not cost money. We could transform the service, save money, and make the patient experience much better. There is a difference from GP-to-GP in the amount of technology they use and I think each should offer the same services.
“With the right governance and security, there is no reason we cannot embrace AI to make healthcare more responsive, connected, and compassionate.”
Steven Grimason
Ursula Mason
That is a choice GPs make based on a practice’s capacity, the services they deliver, and the population they serve. My practice is in an area with very low social deprivation, high health literacy, and digitally enabled patients who are content to book online and receive digital messages from us. I have colleagues in different areas that could not do that. It would not suit their population. With the level of inequalities in Northern Ireland, there may be an argument to be made for using AI to support the concept of using proportionate universalism in respect of access to care. Two people may have the same condition but one’s comorbidities and deprivation level may be worse. Both go on the waiting list at the same time, but in waiting the same time, the more disadvantaged person’s health may have deteriorated perhaps to the point of exclusion from the intervention while the other can stay well and avail of the service they need. The data which informs us on who we should be prioritising is there. If we could do that it would be a game-changer.







