Covid-19: “Turning the final page of this story”

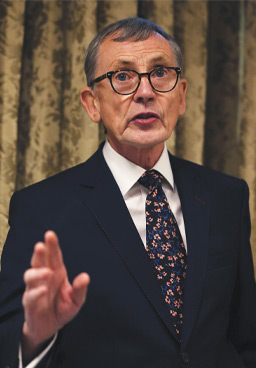
Ciarán Galway discusses the adequacy of Ireland’s public health response to Covid-19 and the necessity of all-island coordination with Gabriel Scally, President of the Epidemiology and Public Health section of the Royal Society of Medicine.
Belfast-born public health specialist Gabriel Scally entered the wider Irish public consciousness having led the Scoping Inquiry into the CervicalCheck Screening Programme. Commencing in May 2018, the work of the Scoping Inquiry concluded in June 2019. Prior to this, in Northern Ireland, Scally assisted as an expert witness and advisor to the chair of the Inquiry into Hyponatraemia-related Deaths, the report of which was published in January 2018.
More recently, throughout the Covid-19 crisis, Scally has been a ferocious critic of the British Government’s lethargic response to the pandemic. In March, reflecting on the lessons learnt from the Ebola outbreaks and applied in the context of Covid-19, WHO Executive Director Mike Ryan advised: “Be fast. Have no regrets. You must be the first mover… If you need to be right before you move, you will never win.”
Echoing Ryan’s sentiments, Scally asserts: “In traditional public health terms, you respond to an infectious disease outbreak with urgency and you make all possible attempts to get ahead of the virus as soon as you possibly can.”
The public health ‘toolbox’ in such scenarios includes: testing to identify the disease if it isn’t immediately obvious; tracing the infection backwards in an attempt to identify the index case; contact tracing to follow spread beyond an infected individual; quarantining as an ancient method of preventing further spread; and disseminating information to tell people that you have found it, thereby raising awareness and determining a potentially wider pattern.
Scally indicates that the countries that have been most effective in their public health response are those that have taken note of, and learnt from, the experience of Severe Acute Respiratory Syndrome (SARS), the zoonotic viral respiratory disease, and thus acted swiftly to introduce social restrictions, shutdown transport systems and introduce border controls, as in South Korea and Vietnam. Most crucially, exemplar countries adopted the principle of finding the virus, tracking it down and killing it.
“Interestingly, many of the locations that have dealt well with it have been islands, not unlike Ireland. New Zealand has done well, Australia has done extremely well, as has Taiwan. Greece has done amazingly well which is interesting given how much its reputation suffered because of its response to and full engagement in creating the economic crisis that affected so many European countries,” Scally says.
Adequate
Acknowledging that it has not been “as good as one would have wanted”, the public health expert regards Ireland’s response as having been “adequate”. In particular, he highlights the failure to halt movement at Irish seaports and airports. “In some ways we are victims of our geographic position and connections. Pursuing some of those measures is countercultural, certainly in a political context, even if it is on public health grounds,” he says.
Another specific criticism Scally makes relates to Ireland’s data systems. Suggesting that some of the Covid-19 data produced has been “first class” and describing the daily briefings as accessible and transparent, he is critical of the guidelines in respect of death registration.
“The length of time within which a death must be registered is three months which is astounding,” he says, adding: “Most people think that deaths should probably be notified to someone official slightly sooner than three months. In Northern Ireland, England and Wales the equivalent figure is five days and in Scotland eight days.”
Consequently, data is very slow in emerging and it was originally thought that Ireland’s performance was much better than the reality. EuroMOMO, a website that provides monitoring for infectious disease outbreaks, initially portrayed Ireland’s excess deaths as remaining flat, for instance. A notification on the site now indicates: “In Ireland, as a result of very significant delays in death registrations during March and April 2020, due to the Covid-19 pandemic, weekly z-scores of excess all-cause mortality do not reflect current Covid-19 (and non-Covid-19) excess mortality in Ireland.”
Lamenting this failing, Scally regards excess mortality comparisons – the number of deaths greater than the average of the previous five years – as the acid test for public health performance.
Consider the shortages of PPE in care facilities. If that’s shielding, then it’s not so much a shield as a sieve.
Care homes
Similarly, Scally is critical of the high mortality rate in Irish care homes, a trend that has been mirrored in several countries. “It is a terrible indictment of the way in which we treat elderly people. Not just the numbers of deaths but the fact that some people are dying, I suspect, without adequate medical and nursing care because the care homes cannot provide it,” he says.
Under normal circumstances, Scally suggests, many of the people dying in care homes would have been admitted to hospital. That didn’t happen. “Personally speaking, in such circumstances, I would like to be very well looked after by expert nurses and doctors who have access to some fairly powerful drugs to help me through that.
“That’s one of my concerns and a second concerns the language used which was about ‘shielding’ and ‘cocooning’ people. In fact, rather the opposite seems to have happened. There seems to have been very little done. Consider the shortages of PPE in care facilities. If that’s shielding, then it’s not so much a shield as a sieve.”
Easing lockdown
At the same time, the public health specialist is satisfied that Ireland has met the criteria set by WHO Director General Tedros Adhanom Ghebreyesus as a guideline for easing lockdown. “We are heading into the final phase now in terms of eradicating the virus from the island, or we should be, if it wasn’t for the North. Just imagine that: if we had no cases on the island, for a few weeks, we could unlock everything. After that, we must be vigilant to pick it up when it pops up. The phases of ending restrictions could be undertaken in an orderly but relatively swift fashion,” he says.
However, Scally is still troubled by the issue of inadequate border control.
“Unless we take control of that situation, we will end up like China where we import many new cases and run the risk of undoing all our efforts. It’s not hard to do. It just requires investment of time and money in quarantining people one way or another. It must be rigorous and universal.
“Otherwise, it makes a nonsense of everyone on the island practising social distancing. People from all parts of the world crammed cheek by jowl in metal tubes for hours and breathing recirculated air and then dispersing all over Ireland upon arrival is just crazy. I recognise fully the problems of having that discussion within the island and with the neighbouring island, but that must be had if we don’t want this to go on, cost more lives and necessitate more disruption,” he says.
North/south harmonisation
Scally has been a vocal proponent of all-Ireland harmonisation of the public health response to Covid-19. He praises the memorandum of understanding (MOU) on public health cooperation on an all-Ireland basis co-signed by Chief Medical Officer Tony Holohan and the North’s Chief Medical Officer Michael McBride as “saying all the right words”.
However, Scally is doubtful whether the Department of Health in Northern Ireland can deliver on the MOU. “It’s not like normal government in Northern Ireland. I do get the feeling that although there is a First Minister and a deputy First Minister, that they don’t have any control over the Health Minister.
“To use my old-fashioned NHS language, it’s not quite clear what the performance management regime is in the North. How can the whole population there and indeed across the island be sure that Northern Ireland’s Department of Health is going to do the job, particularly given some of the ways in which it has been behaving. It has been a very unfortunate episode, I think.”
Single epidemiological unit
Ireland cannot be regarded as two distinct epidemiological units because of the nature of the 499 km-long mile border, Scally contends. “The virus does not respect borders and there are people who live and work on a cross-border basis. We treat Ireland as one epidemiological unit for animal health purposes, so why does it not make sense to treat it as a single unit for human health? To avoid doing so is throwing away our advantage,” he says.
While emphasising that there is only one outbreak on the island of Ireland, the public health expert distinguishes between the responses in either jurisdiction. Following the announcement of school closures in the Republic on 12 March, Scally watched closely over the following weekend as reports filtered in from all across Northern Ireland of people either closing schools unilaterally or refusing to send their children to school.
“The decision that really struck me was made jointly by the heads of the special schools in Belfast to close, irrespective of what the British Government said. It’s a good example of the public leading on the handling of this outbreak and the politicians catching up belatedly,” he reflects.
Following the lead of Westminster, community testing and contact tracing in Northern Ireland had also been abandoned on 12 March, a decision Scally regards as a fatal departure for many people. With the Northern Ireland Executive publishing its strategy for easing lockdown and announcing a revival of testing and tracing, he proposes that a perfect opportunity for mutual assistance had arisen.
We will either get to zero cases on the island and relax many restrictions or, if we don’t have effective border controls and a good testing regime, we will have to wait for a vaccine.
“In the Republic, case numbers are falling and much of the contact tracing capacity isn’t being used. That has been well described in the press. As the numbers decrease, there will be much more intensity in tackling new cases, but there will be spare capacity, for example, in laboratories.
“Meanwhile, the North is trying, without visible evidence of success, to put a case finding, testing, contact tracing and isolation policy in place, with limited laboratory capacity. Here we have a fantastic opportunity for cooperation.”
Overall, Scally feels that very little is standing in the way of an effective all-Ireland response to the ongoing challenges posed by Covid-19. “It merely requires the will on behalf of some people to lay aside their long and no doubt dearly held principles, prejudices and beliefs, focusing instead on ridding the entire island of this virus. It doesn’t matter whether you’re in Ballycastle in County Antrim, Ballina in County Mayo or Bandon in County Cork, it’s in everyone’s interest that there are no cases anywhere on the island.”
Looking ahead
Ireland, as a whole, now faces a choice. “We will either get to zero cases on the island and relax many restrictions or, if we don’t have effective border controls and a good testing regime, we will have to wait for a vaccine,” he contends.
“I haven’t made a big public deal about this next issue because it’s not quite the time, though the time is approaching. There will be a moment when we get through this and there will be a great deal of rejoicing at that time alongside a great deal of grieving for all the people who have died unnecessarily. Personally, I have lost a friend and I hate that. I’m in public health because I hate preventable death. That’s what my career has been; trying to stop people dying unnecessarily. However, as we emerge from this, we must remember how we got here in the first place.”
There is a constant risk from the emergence of new novel viruses and there are always new combinations and strains. Only a single virus needs to get it ‘right’, finding some vulnerability and bypassing our defence mechanisms. Paraphrasing a famous quip, Scally states: “The risk hasn’t gone away you know. It’s still there and will still be there in the future.”
From the first day that follows this crisis, the public health expert asserts, planning must begin for future pandemics. Once the data has been finalised, Ireland, he suggests, must ask itself why its response was not as robust as countries such as Greece, Denmark, Norway or Finland.
Leaning on his experience from the CervicalCheck Inquiry, Scally advises against scapegoating individuals. “It’s an awful response. Rather than doing the hard learning and getting the system right. It’s easy and it’s wrong. We have a fantastic chance to get make sure that this never happens again in Ireland,” he insists.
Optimism
Conceding the inevitability of occasional Covid-19 outbreaks as are being experienced elsewhere such as South Korea, Scally emphasises the importance of vigilance alongside the preservation of some degree of social distancing while necessary and relaxing it when possible.
The experience, he believes, opens opportunities to pursue new thinking in the organisation and delivery of health services. This includes consideration of UK 1948-type action in terms of bringing private hospitals into public ownership.
“I’m very optimistic and I’ll be delighted to see the end of this. It can be done, and the all-Ireland coordination is vital in achieving an organised end to this episode. A joint end. We have to turn the final page of this story at the same time, north and south,” Scally concludes.