Protect Life 2 strategy

Identifying herself as a champion for mental health at the Executive table, Health Minister Michelle O’Neill has pointed to a need for further reform of mental health services going forward. A major catalyst for potential change lies in the Protect Life 2 strategy, currently out for consultation.
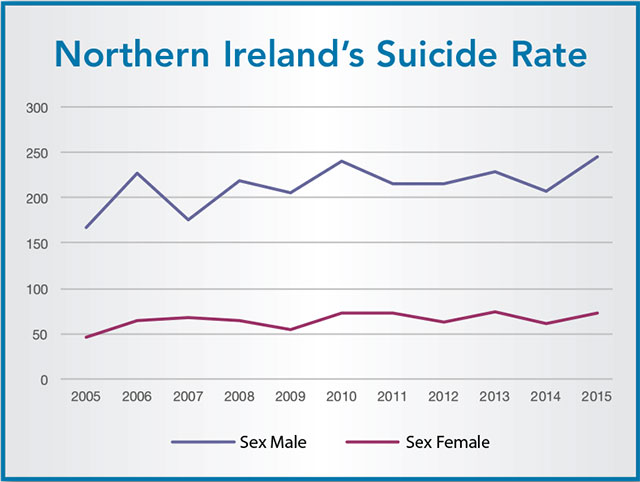
In 2015 the number of suicides in Northern Ireland spiked to 318, the highest it has been since records began back in 1970 and 50 more deaths by suicide than the previous year. Clearly a fresh approach is needed. Protect Life, the original, provided direct investment to tackle suicide of £7 million and while being recognised as contributing to the three year average rate for Northern Ireland remaining unchanged in the last decade, the average suicide rate of 280 deaths each year remains “stubbornly high”.
The new strategy has identified a number of areas for discrete focus in including tackling self-harm, improving initial response to care and recovery of those experiencing suicidal behaviour.
Speaking about the strategy, O’Neill says: “Suicide rates in the most deprived areas here are three times higher than in the least deprived; for self-harm that differential is four times higher. Men continue to be three times more likely to die by suicide than women. As Minister, I am committed to tackling inequalities and I will ensure that resources continue to be focused on reducing these differentials.”
The strategy has identified 10 priorities (see right) for the strategy to target ranging from reduction of self-harm to identifying emerging suicide clusters and reducing risk of further associated suicides in the community. It has also focused on achieving the priorities through core principles for strategic action such as being evidence-based, collaboration with other bodies, co-ordination across government and achieving measurable outcomes amenable to evaluation.
While the strategy has been largely welcomed, some questions have already been raised about the specifics. One omission noted is the lack of any financial detail. In early September, an open letter to the Health Minister signed by more than 600 mental health service users, associated campaigners and supported by a range of MLAs requested that at least 25 per cent of an extra £72 million allocated to the health budget be invested in services. The issue of ring-fencing funding for services working to reduce suicide risk has been long-standing and while the Department will contend that response to the consultation will shape the allocation of finances, service users and deliverers will be keen to ensure that the final version outlines clearly the financial input.
Key to the strategy’s success will be its ability to align with other departmental priorities across government. Sara Boyce, development worker with the charity Participation and Practice of Rights, explains: “Protect Life 2 recognises the clear link between social deprivation and suicide rates – with suicide rates in the most deprived communities being three times the rate experience in the least deprived communities. Yet it fails to tackle two key issues. One is the fact that while mental health accounts for approximately 25 per cent of health cases, it currently receives only 8.5 per cent of the health budget.
“The other is that this strategy is published in the midst of stringent welfare reform cuts currently having devastating impacts on the social security safety nets that many in our most deprived communities rely on. The inescapable fact is that real efforts at suicide prevention will require increased and ring-fenced investment.
“In her response to an open letter from mental health campaigners on funding for mental health services the Minister has indicated that she looks forward to tackling issues in relation to funding of mental health and is committed to the concept of parity of esteem between physical and mental health. The Mental Health Rights Campaign is calling on the Minister to ensure that the Protect Life 2 Strategy and mental health care in general is adequately funded.”
Speaking at the recent launch of two new services by Southern Trust aimed at helping people with mental health issues through their recovery process, the Health Minister reinforced her commitment to prioritising mental health.
“Underpinning the Programme for Government will be my personal commitment to move towards parity of esteem for mental health. This means that mental health would, in time, receive the allocation of attention, effort and resources on a basis which fully meets local needs,” she said.
“This will be a very long-term goal considering the challenging financial position faced by the Executive and the competing priorities right across the Health and Social Care service, but it is the aspiration I have chosen to work towards as a first step in the next phase of improvement in mental health provision.”
The consultation which opened on 9 September will close on 4 November.
10 strategy objectives:
- Fewer people who are in contact with mental health services, die by suicide.
- Reduce the incidence of repeat self-harm presentation to hospital emergency departments.
- Improve the understanding and identification of suicidal and self-harming behaviour, awareness of self-harm and suicide prevention services, and the uptake of these services by people who need them.
- Enhance the initial response to, and care and recovery of, people who are experiencing suicidal behaviour and to those who self-harm.
- Restrict access to the means of suicide, particularly for people known to be self-harming or vulnerable to suicidal thoughts.
- Ensure the provision of effective and timely information and support for individuals and families bereaved by suicide.
- Provide effective support for ‘self-care’ for voluntary, community, and statutory sector staff providing suicide prevention services.
- Enhance responsible media reporting on suicide.
- Identify emerging suicide clusters and act promptly to reduce the risk of further associated suicides in the community.
- Strengthen the local evidence base on suicide patterns, trends and risks, and on effective interventions to prevent suicide and self-harm.





