A predictable crisis

Cuts to public services, staff shortages and an increased winter demand for health services has resulted in an all too predictable ‘crisis’ for the health service writes David Whelan.
In November, the budget announced by then Secretary of State James Brokenshire declared a 5.4 per cent ‘increase’ in health spending for the year 2017/18. The fact is that when inflation is factored in, the budget for health barely stood still.
Added to this is an inaccurate representation of figures. The 2017/18 budget, prolonged due to the impasse at Stormont, was based on mid-year estimates, meaning that it encompased some of the routine monetary round allocations often attained from other departmental underspends and any central government allocations. Comparing this bloated figure with that of the opening position of the previous budget produces an inaccurate comparison and explains how a 5.4 per cent ‘increase’ could be touted.
It is widely understood that Northern Ireland’s health budget requires an annual increase of around 6 per cent to stand still. The unsustainability of these costs prompted the 10-year strategy for transformation of the health service under then Minister Michelle O’Neill, however, the absence of a Northern Ireland Executive for over a year has meant that no major progress on the strategy has been given ministerial sign-off.
Cuts to wider public services have a detrimental impact on quality of life for citizens and ultimately these problems increase the burden being placed on the health service, especially in times of peak demand.
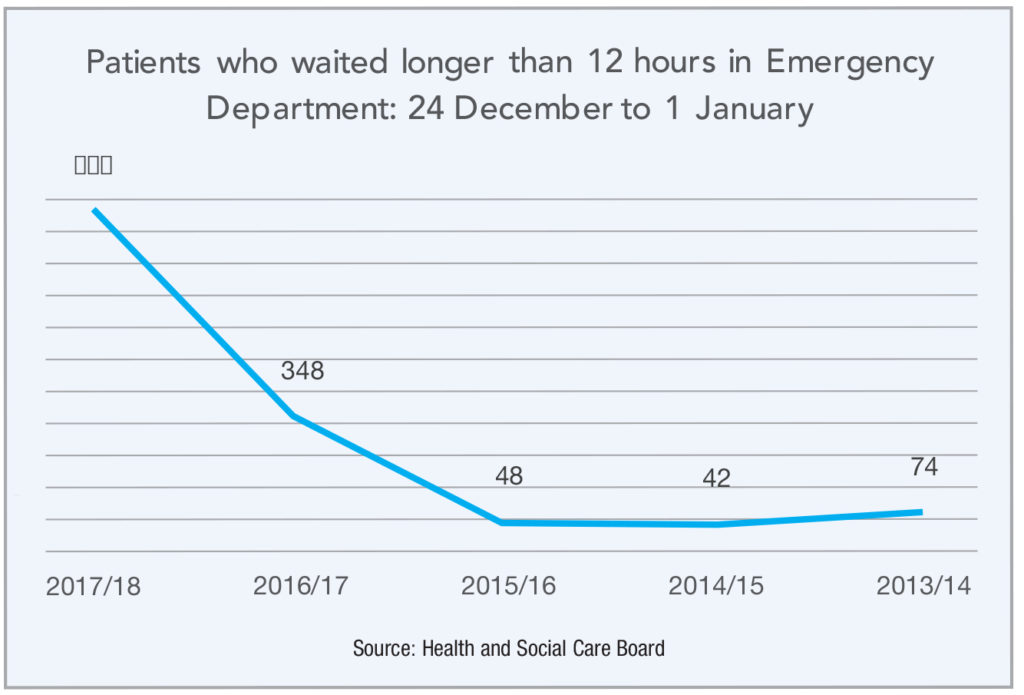
This burden was recently realised in the form of waiting lists in Emergency Departments (EDs) across Northern Ireland over the Christmas period. The BBC obtained statistics that highlighted a more than three-times increase in people waiting in EDs for longer than the 12 hours, compared to the same time last year.
Figures from the Health and Social Care Board showed that 928 patients waited longer than the 12-hour target between 24 December 2017 and 1 January 2018, compared to 348 people over the same time period in 2016/17 and 48 patients for the 2015/16 timeframe.
While the extra pressures being out on the health service by an ageing and growing population have long been mooted, the service in Northern Ireland is still struggling to cope in times of peak demand. As a result, hundreds of non-urgent surgeries scheduled for December were cancelled and routine elective inpatient cases scheduled for the trusts were postponed until the end of January.
This problem has been exasperated by a staffing shortage, in particular amongst nurses. In November, the RQIA formally notified the Department there was a serious nursing shortage across hospitals and community services.
Figures from the Nursing and Midwifery Council (NMC) register show that the number of nurses and midwives leaving the profession are increasing. In 2016/17, 928 left the register compared to 600 during 2013/14. In the first half of 2017/18, 506 had already left the profession.
The Head of the Royal College of Nursing in Northern Ireland, Janice Smyth, indicates that the current condition of the health service is the main cause of “haemorrhaging” from the workforce.
“We can see from the NMC register that the number of nurses who have just had enough and are leaving their jobs is increasing. In fact, they are actually increasing disproportionately compared to the rest of the UK.
“The fact is that nurses here cannot continue to work under the current conditions and we need to do something to address what is happening urgently.”

Smyth added that while poor pay was a major factor in the decision my staff to seek other careers, the main influence on decisions to leave were that providing safe and effective care for patients is becoming “increasingly impossible”.
Adding: “The current pressures, the shortages and workplace environment are becoming unbearable for nurses and they are simply choosing to walk away to protect their own health.”
Some have indicated the need for Stormont to return to alleviate the pressures on the health service, including SDLP leader Colum Eastwood, who described the situation as “shameful”, adding: “The crisis in our healthcare system surely must be a basis for dialogue”. Figures indicate that the health ‘crisis’ is in need of a much longer-term fix than any single minister can provide. The reality is that while the resumption of an Executive may restart work towards health transformation, pressures in the health service will remain for the foreseeable future.